Background: Infections are common among patients with myelodysplastic syndromes/neoplasms (MDS) and acute myeloid leukemia (AML) due to neutropenia, which leads to increase in hospitalization, morbidity and mortality. Antibiotic prophylaxis has been proven to reduce the incidence of infections in oncologic and hematooncologic patients receiving intensive chemotherapies. Accordingly, most hematology and oncology societies advice for its use especially in high-risk patients. These recommendations, however, cannot be directly extrapolated to elderly MDS or AML patients treated with less intensive regimens such as single agent hypomethylating agents (HMA) or low-dose cytarabine (LDC), as controlled prospective randomized trials are not available in this context.
Aim: The aim of this systematic review was to summarize published data on the efficacy and safety of primary antibiotic prophylaxis in patients with MDS or AML treated with non-intensive agents and perform a meta-analysis.
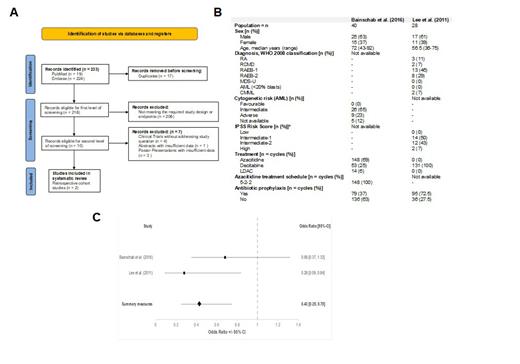
Methods: We performed a systematic review using PubMed and Embase databases on 14th September 2022 without time-restrictions concerning publication data. Inclusion criteria comprised demographics (adult), type of study (retrospective and prospective cohort studies, case control studies, randomized controlled trials), study population (patients with MDS, MDS/MPN or AML), and treatment (hypomethylating agent (HMA), low-dose cytarabine (LDC)). Study outcomes/endpoints included information on efficacy (reduction of infection or fever episodes requiring antibiotic treatment (bacterial, viral, fungal), hospitalizations, intensive care unit admissions or leading to dearth) and safety (antibiotic side-effects and resistance) of primary antibiotic prophylaxis. Meta-analysis was performed and odds ratios with 95% confidence intervals shown in a Forrest Plot.
Results: From 233 screened studies, we identified no randomized or prospective studies and only two retrospective studies with 68 patients and 346 treatment cycles that matched our inclusion/exclusion criteria. ( A). One study included AML (n=40, Bainschab et al, 2016) and the other MDS patients (n=28 , Lee et al, 2011). Patients recived primary antibiotic prophylaxes in 79/215 (25%) and 95/131 (72.5%) treatment cycles, respectively (B). The antibiotics used included fluorquinolones (92.5% and 95%), penicillins (6.5% and 0%) and cephalosporins (1% and 5%). Infections episodes were reported in 53/215 (25%) and 15/131 (11%) treatment cycles. A meta-analysis of the selected studies suggests a significant benefit in reducing the incidence of infection or febrile episodes (OR 0.43 [0.25-0.75], p<0.003) with potential reduction in hospital admission, especially in patients with low ANC (< 0.5 G/l). As additional risk factors for infectious complications we identified severe cytopenia (grade ≥3) in at least one lineage, earlier therapy cycles, transfusion dependency, increased LDH and high Charlson Comorbidty Index. Data regarding the safety and tolerability of antibiotic prophylaxis was not available.
Conclusion: Our investigation with only few eligible studies, patients and treatment cycles underlines an unmet need for prospective controlled trials in this field.Our systematic review with meta-analysis suggests a significant benefit of antibiotic prophylaxis in MDS and a tendency in AML patients undergoing single agent HMA or LDC treatment. Those individuals with high-risk features seem to have the greatest benefit. Prospective, controlled and randomized trials are, however, lacking and should be encouraged, even more as combinations with venetoclax are becoming the standard of care in AML and potentially also in MDS with higher risk of neutropenic infekctions.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal